Two new reviews of research on the outcomes of treatments for chronic back and neck pain are a call to action to prioritize evidence-based, conservative care.
This spring, the American Academy of Neurology completed a review of research on epidural steroid injections for chronic back pain. It concluded that the procedure offered only a limited reduction in back pain or disability.
A new Clinical Practice Guideline in The BMJ (formerly the British Medical Journal) went further. It powerfully critiqued multiple invasive interventional procedures, such as spinal injections and nerve ablations, for chronic spine pain. The committee reported that many commonly performed procedures for non-cancer chronic spine pain offer little to no proven benefit. Those procedures, it said, should be abandoned in routine care.
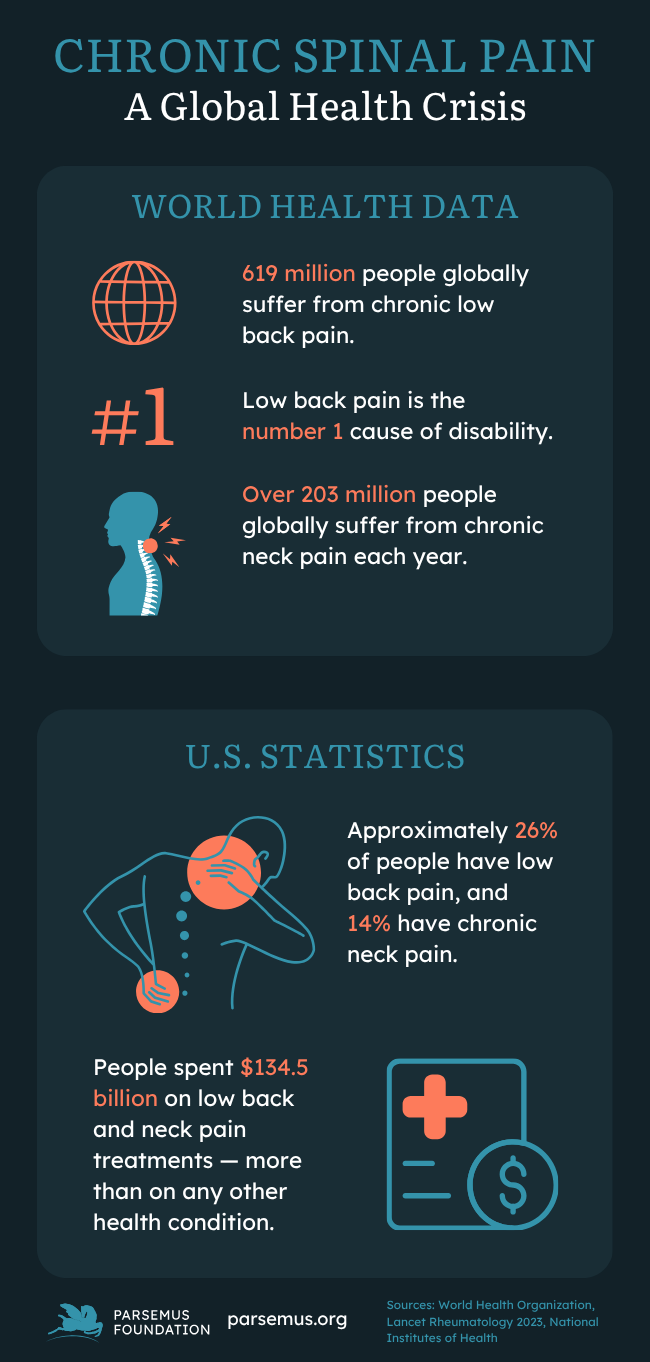
Chronic spine pain: a growing problem
Chronic spinal pain—including conditions like persistent low back and neck pain—is a public health crisis. According to the World Health Organization, 619 million people around the globe suffer from chronic low back pain. Over 203 million people suffer from chronic neck pain each year. In the U.S., approximately 26% of people have low back pain, and 14% have neck pain.
Spine pain is the leading cause of disability worldwide. It accounts for staggering healthcare costs, estimated at over $134 billion annually in the U.S. alone. In the search for relief, patients and providers have increasingly turned to invasive interventional procedures, such as spinal injections and nerve ablations.
Weighing risks against benefits
The American Academy of Neurologists studied the commonly used epidural steroid injections for spine pain. Methodologists first reviewed studies on the efficacy of these procedures and selected 90 randomized controlled studies for their systematic review. Then, a panel of experts in epidural steroid injections interpreted the evidence regarding clinical practices.
The findings, published in Neurology, concluded that short-term benefits were limited for epidural steroid injections in reducing pain and disability in treating cervical and lumbar radiculopathies (compressed nerves) and possibly in lumbar spinal stenosis (narrowed spinal canal).
“In our review, studies show epidural steroid injections may have limited efficacy. They may modestly reduce pain in some situations for up to 3 months and reduce disability for some people for up to 6 months or more.”
— Carmel Armon, MD, Professor of Neurology, Loma Linda University School of Medicine

A strong statement against spine pain interventions
The new guideline, published in The BMJ, took a broad look at popular interventions for spine pain and issued strong recommendations against their routine use. Developed by an international panel of experts, this systematic review included:
- Epidural injections (administering local anesthetic, steroids, or both)
- Facet joint injections and sacroiliac joint injections (joint-targeted injections)
- Radiofrequency ablation (using heat to temporarily silence pain-transmitting nerves)
The guideline’s most striking finding is the panel’s strong recommendation against the use of many common procedures for a significant portion of the patient population—specifically, adults with chronic axial spine pain (pain localized to the midline of the spine, like persistent non-radicular low back pain). For these individuals, the guideline determined that joint-targeted injections, which aim to target specific pain generators in the joints of the spine, should not be offered outside of a clinical trial.
The expert panel concluded that the risks, costs, and burden of these interventions generally outweigh any meaningful chance of success. They asserted that nearly all well-informed patients would likely decline these treatments. This means they should not be part of standard clinical practice.
Controversy over the findings
The panel’s report met with mixed results. Many physicians and organizations disagreed with the results and recommendations against interventional spine pain treatments. A response to The BMJ publication on behalf of 34 professional societies, representing physicians worldwide who treat patients with chronic pain, was notable. It expressed serious concerns about the study’s methodology and the lack of sufficient high-quality randomized trials to make broad recommendations. It also indicated that the panel didn’t fully consider the patient’s preference in the decision-making process. Furthermore, it argued that these recommendations could lead to reduced healthcare coverage.
Implications for evidence-based spine pain treatments
Given these findings and the controversy about them, patients may wonder why the procedures are so commonly used. Revenue is likely one reason, as a single procedure may cost $1,000 or more. Another reason may be the training that physicians specializing in pain treatment undergo, which focuses on the use of anesthetics. The promise of immediate relief from pain may also influence patients’ decisions to choose these interventions.
Experts agree that chronic spine pain care should focus on multidisciplinary approaches with high-certainty evidence of benefit. Pain treatments that have shown benefit include:
- Physical therapy and structured exercise programs
- Psychological interventions (such as cognitive behavioral therapy)
- Appropriate non-opioid pharmacotherapy
Unlike interventional treatments, these options may require patient training and support, involvement and effort from the patient, and long-term monitoring. Patients with chronic pain should also be involved in shared decision-making, ensuring that they understand the rigorous evidence before consenting to procedures.
A focus on evidence-based medicine
The Parsemus Foundation believes that the more you know, the better you’re able to navigate healthcare systems. We support the use of evidence-based information to guide healthcare decisions. We provide summaries of scientific studies to help individuals make informed decisions for themselves, their families, and their pets.
If you suffer with spine pain, carefully consider the best treatment options in consultation with your physician, keeping in mind that non-invasive options may offer positive results.
You can learn more about finding evidence-based health information here.