Please note: This is an archived project that is not currently being updated.
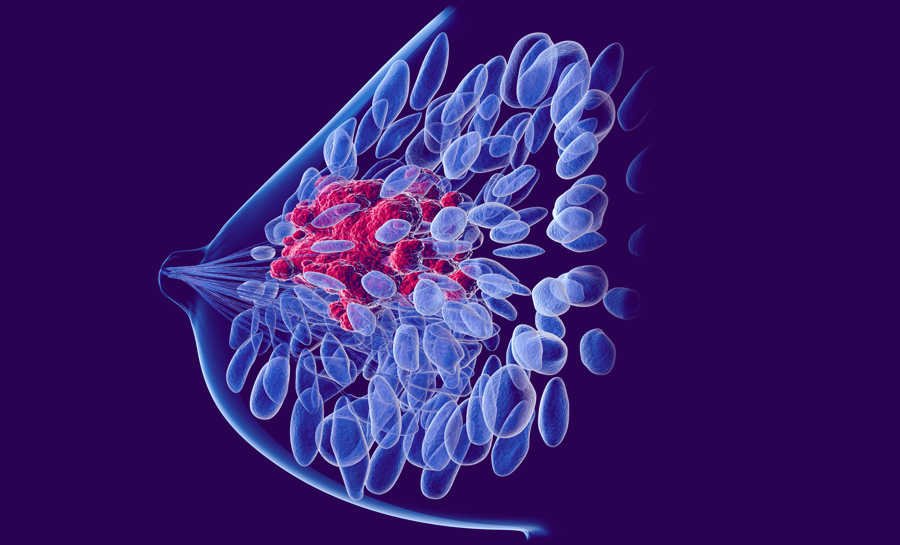
Ductal carcinoma in situ (DCIS) is cells from the milk ducts that have become cancerous but have not spread. DCIS diagnoses have become much more common with increased mammography. Doctors have questioned the current aggressive treatment options, and intraductal evaluation and treatment options may be better options.
PROJECT
Breast Cancer
Prevention
HUMAN HEALTH
PROJECT
Breast Cancer
Prevention
HUMAN HEALTH
Project summary
Background
- DCIS diagnoses have increased greatly due to increased rates of mammography.
- Surgery, radiation, and hormone therapy — the standard treatment for DCIS — have significant side effects and no impact on long-term survival.
Key points
- Since only a portion of DCIS cases progress to invasive breast cancer, treatment plans need to be tailored to the individual by carefully evaluating risks on a case-by-case basis.
- More research on less invasive, intraductal approaches will help provide additional options for those diagnosed with DCIS.
Parsemus' role
- The Parsemus Foundation advocates for non-invasive and simple approaches to complex health issues, and supports the intraductal approach for preventing, evaluating and treating breast cancer.
- To support individualized medicine, we provide educational information on DCIS so that informed health decisions can be made.
Other women’s health projects
Doctors call for less invasive methods to treat ductal carcinoma in situ (DCIS)
The Parsemus Foundation encourages research on simple approaches that could have a big impact, including the intraductal approach to early breast cancer — preventing, or eliminating, early cellular changes in the milk ducts (where the great majority of breast cancers start). When these changes are detected, the condition is called ductal carcinoma in situ (DCIS) — the most common noninvasive lesion of the breast. With mammography becoming standard practice, the diagnosis of DCIS has skyrocketed, now accounting for over 20% of breast cancer diagnoses. Surgery, radiation, and hormone therapy are standard therapies, despite the fact that only a portion of DCIS cases progress to invasive cancer.
But scientists and physicians have been increasingly questioning the aggressive traditional treatment of DCIS. This pre-cancerous condition may be over-diagnosed and over treated in the U.S., and clinical trials have shown that while radiation and hormone therapy can reduce the risk of invasive recurrence, they have no effect on survival. There has been a call for tailoring the treatment to the woman, and carefully evaluating risks. Newer molecular profiling may serve to more effectively predict whether the condition will progress (see reviews by Feinberg and colleagues, 2018 and Barrio & Van Zee, 2017, and information on molecular evaluation by Nofech-Mozes et al, 2019).

Intraductal treatment of DCIS for breast cancer prevention and evaluation
Increasing evidence suggests that evaluating and even treating DCIS through the breast ducts can be an effective nonsurgical alternative. Dr. Susan Love has been an advocate of the intraductal approach for years, with research studies focused on mapping the breast ducts with 3D ultrasound. Ductal lavage, ductoscopy, and intraductal infusion of therapeutic agents may enhance breast cancer treatment. See details below.
- Intraductal lavage involves flushing the mammary ducts and collecting the fluid for analysis of the cells. This method is becoming more common, especially for women at high risk of breast cancer. While the sensitivity required to detect abnormal cells visually is not ideal, evaluation of molecular indicators in the fluid is proving to be a useful diagnostic tool.
- Mammary ductoscopy (threading a tiny endoscope into the breast ducts) is a noninvasive method that can help to visualize and sample lesions. Ductoscopes have been developed with fiber optics to aid visualization. This method can also be used to guide lumpectomy surgery, which helps to avoid the additional surgeries that may be required when lesions are missed with traditional methods.
- Intraductal infusion is a method to put therapeutic agents directly into the duct system, where most breast cancers originate. It’s less likely to cause systemic toxicity since the physician is targeting a specific area. A number of clinical trials of intraductal chemotherapy have indicated the safety and feasibility of this method for breast cancer prevention.
Take Action on Breast Cancer Prevention
If you or someone you know has been diagnosed with DCIS, review the references here to learn more about the risks and benefits of different treatment options. Be sure to ask your physician about molecular profiling (to determine if you are in a low-risk group) and intraductal approaches that might help you avoid more aggressive treatment options.