Vaccines can offer broad protection beyond the diseases that they were meant to target. This is called the non-specific effects of vaccines. The beneficial effects of live vaccines can be used to inform vaccination policies and address diverse health issues.
PROJECT
Non-Specific Effects
of Vaccines
HUMAN HEALTH
PROJECT
Non-Specific Effects
of Vaccines
HUMAN HEALTH
Project summary
Background
- Childhood mortality is high in many parts of the world, especially in low-income countries. According to UNICEF, in 2021, 1 in 14 children in sub-Saharan Africa died before reaching their fifth birthday — 15 times higher than the risk for children born in high-income countries.
- Vaccinations are a way to protect children — and adults — from particular diseases. However, to increase the positive impact of vaccines, the type and timing of the vaccination schedule is critical.
Key points
- Routine vaccinations are a key part of protecting the health of children.
- Our understanding of the non-specific effects of live vaccines has grown tremendously in the past decade. For example, scientists understand that there is a greater impact of these non-specific effects on females as well as an important vaccine sequence to consider.
- Updated vaccination policies that take into consideration the positive non-specific effects that live vaccines can have could greatly reduce childhood mortality in low-income regions.
- More emphasis on studies aimed at leveraging existing vaccines to fight new viruses, such as COVID-19, and other diseases like cancer is needed.
Parsemus' role
- The Parsemus Foundation supports research on the non-specific effects of vaccines to improve human health. We supported a clinical trial on the impact of the live MMR (measles, mumps, rubella) vaccine to protect against COVID-19.
- The Optimmunize Conference brings together scientists who study the beneficial non-specific effects of vaccines. We supported the 2022 conference and assisted with publicity about their work.
Topics
- Vaccines 101
- Non-specific effects of vaccines
- A call for improving the vaccine strategy for newborns
- Trained innate immunity and the benefits of attenuated vaccines
- What is the future for trained innate immunity and beneficial non-specific effects?
- Take action on non-specific effects of vaccines
- Additional resources
Other human health projects
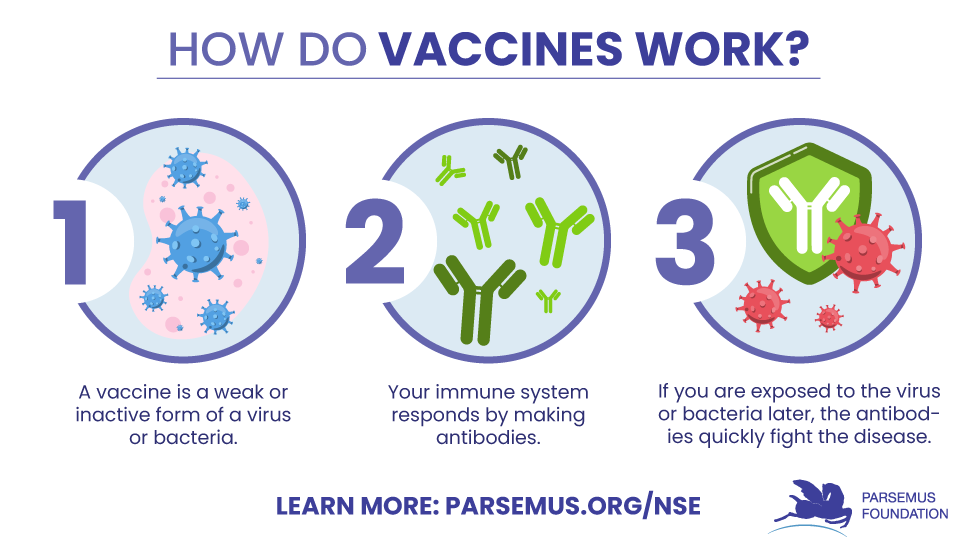
Vaccines 101
Vaccines are given to help your immune system fight off infections and diseases. They work by priming your immune system so it will recognize an intruder virus or bacteria and be able to remove it.
A vaccine is a weak or inactive form of a disease and is usually given by injection. Your body sees it as an invader and launches an attack by creating antibodies to the disease to kill it. This prepares your body to recognize the disease (and does not usually make you ill). Then, if you’re exposed to the disease later, the antibodies remember it and defend against it.
We usually think of a vaccine as being targeted to a specific disease, like the flu. Some vaccines are killed or inactivated. Other vaccines are live or “attenuated,” meaning they cannot replicate enough to cause illness in our bodies but can still be recognized by the immune system.
Non-specific effects
of vaccines
Vaccines may have influences beyond the disease they target. These “non-specific effects” of vaccines can be positive or negative. Some vaccines can be successful in helping the immune system to fight other pathogens besides those it was created to target. Live vaccines often have beneficial effects by fighting non-target diseases. For example, the measles vaccine can also protect against sepsis (a life-threatening response to infection). This non-specific effect can be very powerful. Researchers have found that live vaccines for smallpox, tuberculosis (BCG), polio, and measles (or MMR) can actually reduce child mortality, beyond the protection they give for those diseases.
On the other hand, non-live (killed) vaccines may have the opposite effect. The non-live vaccines — such as DTP (diptheria-tetanus-pertussis) vaccine, hepatitis B vaccine, inactivated polio vaccine, malaria vaccine, H1N1 influenza vaccine — are effective against the target diseases but can increase the chance of unrelated infections.
Studies in low-income countries indicate that these non-live vaccines may increase mortality in children because the increase in pneumonia and sepsis outweighs the benefits of fighting the target diseases.
In high-income countries, where child mortality is lower, similar findings have occurred. For example, a study in Denmark found that hospitalization of children for unrelated infections was reduced by recent live measles vaccination. And the non-specific effects of vaccines occur in adults as well. A randomized placebo-controlled human challenge study found that adults vaccinated with the tuberculosis vaccine were protected against an experimental infection.
The non-specific effects of vaccines are greater in females than males
The non-specific effects of vaccines are greater in females than males. This applies to both the protective effects of live vaccines and the detrimental effects of non-live vaccines. In Africa, non-live vaccination for malaria was found to double mortality rates in girls. However, the non-specific effects of live tuberculosis vaccine had greater beneficial effects on mortality for girls than for boys.
Timing is important
How can we reduce the negative impact of non-live vaccines? Luckily, scientists found that the most recent vaccine given has the strongest non-specific effects. So, when children receive a number of different vaccines, the best way to reduce the negative effects of non-live vaccines is to be sure that vaccines are scheduled to give a live vaccine after the non-live vaccine. In Denmark, children who were given the live measles, mumps, and rubella vaccine after the non-live vaccine had a lower rate of hospital admissions for any infections. In the U.S. researchers found a similar outcome. Children had a lower risk of non-target disease hospitalizations when the last vaccine received was a live vaccine as compared to a non-live vaccine.
A call for improving the vaccine strategy for newborns
- All children in Africa should receive the tuberculosis vaccine at birth to boost the infant’s immune system, which can reduce neonatal mortality by 33%.
- Oral polio vaccine should not be phased out. This live vaccine has helped to reduce child mortality in low-income countries.
- Children should be given a live vaccine shortly after receiving non-live vaccines. For example, they should be given the measles (live) vaccine after the DTP (non-live diphtheria, tetanus, pertussis) vaccine.
By simply changing the vaccination policies as to the sequence and types of vaccinations given to children in low-income countries, it is estimated that approximately 1 million lives could be saved each year. These same concepts could also improve outcomes for children in mid- and high-income countries.
The way vaccines are tested, approved, and regulated should also consider non-specific effects to enhance the positive impacts on overall health (see this publication for specific suggestions).
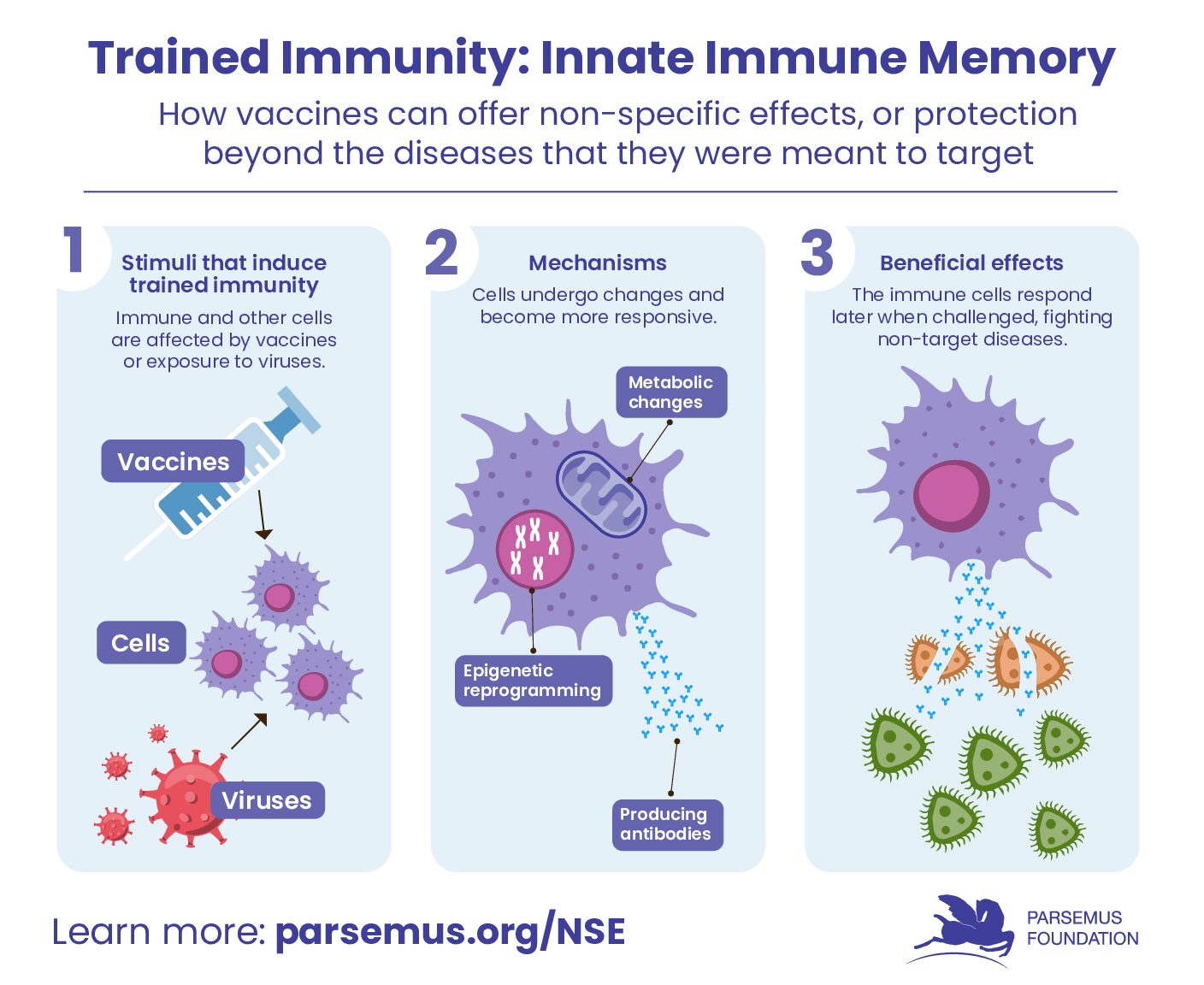
Trained innate immunity and
the benefits of attenuated vaccines
For those wanting more details on how a vaccine can have non-specific effects, we need to introduce the concept of “trained innate immunity.” Trained immunity refers to the ability of the innate immune system to form immune memory and provide long-lasting protection against foreign invaders. Basically, a vaccine kicks the immune system into high gear so it is better able to fight many disease organisms, and therefore provide broader protection.
This process involves changing the innate immune cells by internal or external attacks (such as by a vaccine or virus), resulting in myeloid cells being metabolically and epigenetically reprogrammed. The cells return to a non-activated state but then respond if challenged again later.
Definition:
Epigenetic reprogramming means that environmental factors such as diet, infectious disease, or vaccination can influence how the genes of a person are expressed (whether a specific gene is turned on or turned off) without changing the actual DNA sequence of the genes themselves.
Live viral and bacterial vaccines (such as tuberculosis, measles, oral polio, and influenza) have been shown to induce trained immunity with protection against non-target diseases. See this article for more details.
What is the future for trained innate immunity and beneficial non-specific effects?
Take Action on Non-Specific Effects of Vaccines
Understanding the different types of vaccines and how they work is an important part of healthcare, especially for children. The knowledge we have now about the importance of the scheduling of live attenuated vaccines can help to create policies that enable the most positive impact of non-specific effects.
Additional resources
TedXAarhus Video: “How vaccines train the immune system in ways no one expected”
Video: Christine Stabell-Ben “How vaccines train the immune system in ways no one expected” TEDxAarhus 2018.
Podcast: “Vaccines: A tale of the unexpected” BBC Health Check Mar 1, 2023.
Podcast: “Vaccines: A tale of the unexpected” BBC HealthCheck Mar 1, 2023.
Further reading and links
Aaby P, Netea MG, Benn CS. (2023). Beneficial non-specific effects of live vaccines against COVID-19 and other unrelated infections. Lancet Infect Dis 23(1): e34–e42. (Full text)
Aaby P, Benn CS, Flanagan KS, et al. (2020). The non-specific and sex-differential effects of vaccines. Nat Rev Immunol 20(8): 464–470. (Full text)
Arts RJW, Moorlag SJCFM, Novakovic B, et al. (2018). BCG vaccination protects against experimental viral infection in humans through the induction of cytokines associated with trained immunity. Cell Host Microbe 10;23(1):89-100.e5. (Full text)
Bardenheier BH, McNeil MM, Wodi P, et al. (2017). Risk of non-targeted infectious disease hospitalizations among U.S. children following inactivated and live vaccines, 2005–2014. Clin Infect Dis 65(5):729-737. (Full text)
Benn CS, Fisker AB, Rieckmann A, et al. (2020). Vaccinology: time to change the paradigm? Lancet Infect Dis 20(10):e274-e283. (Abstract)
Benn CS, Amenyogbe N, Björkman A, et al. (2023). Implications of non-specific effects for testing, approving, and regulating vaccines. Drug Safety 46:439–448. (Full text)
Fedrizzi EN, Girondi JBR, Sakae TM, et al. (2022). Efficacy of the measles-mumps-rubella (MMR) vaccine in the reducing the severity of Covid-19: An interim analysis of a randomised controlled clinical trial. J Clin Trials 12(15) No: 1000004. (Full text)
Klein SL, Shann F, Moss WJ, et al. (2016). RTS,S malaria vaccine and increased mortality in girls. ASM Journals mBio 7(2). (Full text)
Moorlag SJCF, van Deuren RC, van Werkhoven CH, et al. (2020). Safety and COVID-19 symptoms in individuals recently vaccinated with BCG: a retrospective cohort study. Cell Rep Med 25;1(5):100073. (Full text)
Murphy DM, Cox DJ, Connolly SA, et al. (2023). Trained immunity is induced in humans after immunization with an adenoviral vector COVID-19 vaccine. J Clin Invest 133(2):e162581. (Full text)
Netea MG, Domínguez-Andrés J, Barreiro LB, et al. (2020). Defining trained immunity and its role in health and disease. Nat Rev Immunol 20(6): 375–388. (Full text)
Netea MG, Joosten LAB. (2024). Trained innate immunity: Concept, nomenclature, and future perspectives. J Allergy Clin Immunol 154(5):1079-1084. (Full text)
Omar M, Muhsen K. (2021). A narrative review of nonspecific effects of pediatric vaccines on child mortality and morbidity. Hum Vaccin Immunother 17(12): 5269–5283. (Full text).
Schaltz-Buchholzer F, Berendsen M, Roth A, et al. (2020). BCG skin reactions by 2 months of age are associated with better survival in infancy: a prospective observational study from Guinea-Bissau. BMJ Glob Health 5(9):e002993. (Full text)
Sinha S, Ajayababu A, Thukral H, et al. (2022). Efficacy of Bacillus Calmette–Guerin (BCG) caccination in reducing the incidence and severity of COVID-19 in high-risk population (BRIC): a Phase III, multi-centre, quadruple-blind randomised control trial. Infect Dis Ther 11:2205–2217. (Full text)
Sørup, Benn CS, Poulsen A, et al. (2014). Live vaccine against measles, mumps, and rubella and the risk of hospital admissions for nontargeted infections. JAMA 311(8):826-35. (Full text)
Yamazaki-Nakashimada MA, Unzueta U, Gámez-González B, et al. (2020). BCG: a vaccine with multiple faces. Hum Vaccin Immunother 16(8). (Full text)