Project Summary: Hormones for Menopause
Menopause can have significant physical and mental impacts on women at midlife. In the past, it was barely discussed. But today women expect accurate information on how best to manage their health. Hormone replacement for menopause (or menopause hormone therapy) can effectively address vasomotor and other symptoms and improve lifelong health. Yet most women stopped hormone therapy 20 years ago when a clinical trial reported increased breast cancer risk. Today, we know that the type and timing of hormones for menopause makes all the difference to risk analysis. This site offers resources so that you can learn more about hormones for menopause, and focuses on two topics that are often neglected: testosterone for women and hormones after breast cancer.
For more information on menopause hormone therapy, see Additional Resources below for websites and key scientific publications.
- While all women go through menopause, until recently it has garnered little attention.
- Women have not had access to factual information about hormones for menopause to treat symptoms, which range from mild to severe.
- The 2002 announcement of a link between the hormone replacement used in the Women’s Health Initiative clinical trial and breast cancer caused most women to stop taking hormones for menopause.
- Women are active well past the age of menopause, and are now demanding better access to information and relief from menopausal symptoms.
- Research in the last 20 years has shown that menopause hormone therapy can not only improve vasomotor symptoms, such as hot flashes, but also can have important long-term health benefits when used properly.
- Many physicians, including gynecologists, are not well-trained about menopause or hormone therapy, making it difficult for mid-life women to get accurate information to make health decisions.
- The Parsemus Foundation has a history of supporting research and evidence-based information on women’s health, menopause and menopause hormone therapy.
- Support was provided to initiate a new nonprofit organization called the Menopause Hormone Project that’s focused on providing accurate information about hormones for menopause to the public and physicians.
- This site provides information on two misunderstood and often controversial topics: testosterone for women and hormones after breast cancer.
Project Topics
The physical and psychological effects of menopause
Menopause occurs as the female reproductive cycle slows down and the ovaries make fewer hormones. The timing differs for each woman, but usually begins around the mid-40s and menopause is officially reached after you miss your period for 12 months (at the average age of 51 years). The effects of changes in hormone levels can start years before menopause (“perimenopause”) and last for years after menopause (“postmenopause”).
In addition to cessation of menstruation, menopause is related to an increase in physical and emotional changes. Each woman’s experience differs, but may include:
- Vasomotor symptoms: Hot flashes, night sweats and/or cold flashes
- Vaginal dryness or atrophy that causes discomfort during sex
- Urinary urgency, frequency, or incontinence, or urinary tract infections
- Difficulty sleeping and insomnia
- Emotional changes, mood swings
- Dry skin, dry eyes, or dry mouth
- Breast tenderness
- Worsening of premenstrual syndrome
- Irregular periods or periods that are heavier or lighter than usual
- Racing heart, palpitations
- Headaches
- Joint and muscle aches and pains
- Changes in libido
- “Brain fog” — difficulty concentrating and with recent memory
- Weight gain
- Hair loss or thinning
In addition to the menopause symptoms, there are long-term implications of the loss of hormones. Women experience a significant increase in heart disease, osteoporosis, stroke, and other ailments around menopause.
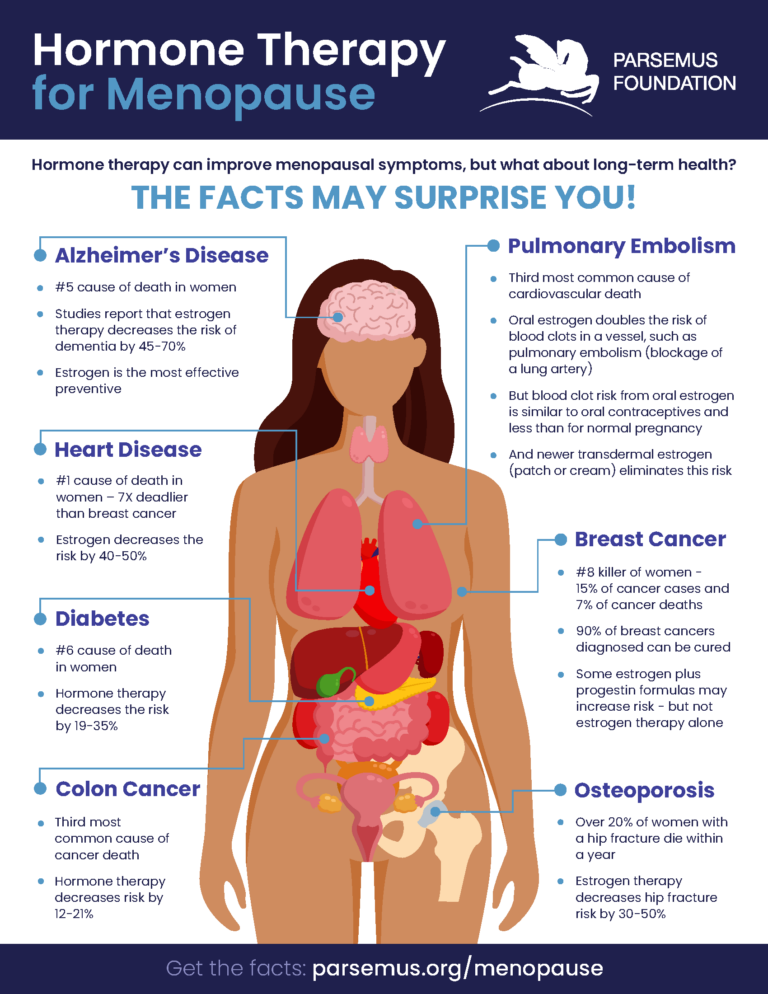
Estrogen is a hormone that affects many areas of the body. Importantly, it influences bone and lipid metabolism, cardiovascular health, cognition, and sexual function. Postmenopausal estrogen replacement therapy is known to alleviate vasomotor symptoms like hot flashes, have a positive effect on the prevention of osteoporosis, and result in improved serum lipid profiles and reduced cardiovascular disease factors if started soon after menopause. Click on the infographic above for more information on diseases prevalence and those that are improved with menopause hormone therapy.
The misunderstood Women’s Health Initiative Study
Despite the positive effects of hormone replacement therapy, in 2002 the results of the Women’s Health Initiative (WHI) Study reported that hormone therapy for women was related to a 24% increased risk for invasive breast cancer, with no major beneficial effects against cardiovascular disease, stroke, and thromboembolic diseases. Within three months of the publication of this report, 63% of women stopped taking hormone replacement therapy.

“The misinterpretation of the WHI (Women’s Health Initiative) Study has led to an irrational fear of female hormone replacement, both by the general population and medical professionals.” Deli et al., 2020.
“During the 20 years since its initial publication, the
WHI investigators have walked back almost all the negative conclusions.” Bluming, 2022.
The problem was that the WHI study used oral conjugated equine estrogen and synthetic progesterone in women long after menopause onset (the average age of participants was 63 years). For women aged 50 to 59 years in the WHI study, hormone therapy did not increase cancer or cardiovascular deaths after a median of 18 years’ follow-up compared with women not taking hormones. With estrogen alone, mortality related to breast cancer, Alzheimer’s disease, or dementia was reduced!
Nonetheless, the fear of breast cancer from hormone replacement therapy became so widespread that misinformation is still common 20 years later. And worse, most physicians practicing today received little if any training on menopause or menopause hormone therapy. This situation has resulted in a lack of credible health information for women at midlife.
The right hormones at the right time
The North American Menopause Society indicates that the risks of hormone therapy differ depending on type, dose, duration of use, route of administration, timing of initiation, and whether a progestogen is used. Evaluating whether menopause hormone treatment is appropriate for you requires an individual assessment with a knowledgeable physician to evaluate your symptoms as well as personal and family health history. And while more research is needed on menopause hormone therapy, we understand that the type and timing of hormones is important.
Menopause hormone therapy initiated soon after menopause has very few risks
Menopause occurs at an average age of 51, but can vary widely between women. As we know from the Women’s Health Initiative study described above, the type and timing of hormone therapy are related to its benefits. Hormone therapy is best initiated around the time of menopause. For women aged 50 to 59 years in the WHI study, hormone therapy did not increase cancer or cardiovascular deaths, and with estrogen alone, mortality related to breast cancer, Alzheimer’s disease, or dementia was reduced. Additional research has indicated that hormone replacement therapy started in women under 60 years of age was related to less cardiovascular disease and lower mortality during the study period.
Micronized progesterone for women with a uterus, transdermal estrogen, and intravaginal estrogen
There are many forms of hormones. For example, the WHI trial used an oral estrogen derived from horse urine (conjugated equine estrogen) and a synthetic progesterone (medroxyprogesterone acetate). Estradiol and progesterone are formulations that are biologically the same as the hormones in your body, and some research indicates they have fewer health risks. For example, transdermal estradiol does not appear to increase the risk of pulmonary thrombosis (blood clot in the lung) as found for oral estrogen. For women with a uterus, progesterone is necessary to keep the lining of the uterus healthy. Micronized progesterone may have less risk for venous thromboembolism than other progestins. Intravaginal estrogen treatments are effective for genitourinary symptoms (such as urinary tract infections, vaginal dryness, and sexual dysfunction). This route of administration does not change estradiol levels in the body above the normal postmenopausal range with long term use. Intravaginal estrogen also does not increase the risk of coronary heart disease, stroke, thromboembolism, colorectal cancer, endometrial cancer, breast cancer, or breast cancer recurrence with their use.
Don’t forget testosterone
Many people who think of testosterone as a “male” hormone are surprised to find that women normally produce 3-4 times more testosterone than estrogen! Testosterone is linked to sexual desire and arousal, but also to mood, energy level, and general wellbeing. It works with estrogen to maintain bone and muscle mass. Testosterone level decreases over a woman’s lifespan. Despite its importance, testosterone deficiency in women has received very little research attention and few products address female testosterone replacement. In all countries (other than Australia), there are no licensed testosterone products available for women. Usually, a smaller dose of an approved transdermal male formulation (prescribed off-license) is recommended. But many physicians do not support treating testosterone deficiency in women. This all stands in sharp contrast to the attention paid to “Low T” in men.

Some believe that supplementing with testosterone causes side effects such as excess hair growth, breast cancer, or cardiovascular disease. But testosterone therapy aims to treat a deficiency, while keeping levels within the physiological range, which should not result in “masculinization.” Research on testosterone therapy in women is limited, but shows promise in improving sexual function and urinary tract health, as well as benefiting bone density, muscle mass, mood, energy, and cognitive function. Studies of transdermal testosterone have not found increased incidence of heart disease, stroke, venous thromboembolism, or cardiovascular death.
Testosterone has not been associated with increased cancer risk and may even reduce the chance of developing breast cancer. Some research also reports that testosterone can have anti-cancer effects when used with traditional breast cancer treatments (see Hormones after breast cancer section below).
The International Society for the Study of Women’s Sexual Health provides standards for prescribing testosterone to women.
Hormones after breast cancer
Women with estrogen-receptor positive breast cancer often receive anti-estrogen treatment, such as tamoxifen or aromatase inhibitors. The resulting sudden reduction in estrogen levels may cause severe menopausal symptoms. Understandably, physicians and breast cancer survivors are particularly cautious about hormone therapy to treat these symptoms. But can hormone therapy help the thousands of women suffering from anti-estrogen treatment?

The good news is that almost all studies of hormone therapy after breast cancer have reported no change in cancer recurrence, and no studies found a negative effect on mortality — in fact quite the opposite! See this thorough review for more details. Estrogens may even cause breast cancer cell death after a period of treatment with anti-estrogens. For example, a randomized trial in women with advanced breast cancer who developed resistance to aromatase inhibitors found that daily estrogen helped prevent recurrence and improve breast cancer sensitivity to treatment.
Low-dose intravaginal estrogen therapy can address genitourinary symptoms of menopause — such as vaginal dryness and urinary tract infections — and existing research shows no impact on breast cancer recurrence. The American College of Obstetricians and Gynecologists has endorsed its use.
Emerging research also reports that testosterone can have positive effects when used in addition to traditional breast cancer treatments such as tamoxifen or aromatase inhibitors. The Parsemus Foundation supported research in a mouse model of breast cancer that reported that bioidentical estrogen, progesterone, and testosterone resulted in reduced breast tumor growth and increased cognition, physical activity, and cardiovascular and bone health. Used alongside aromatase inhibitors, estradiol and progesterone improved cardiac and bone health in the mice without promoting breast tumor growth. See our webpage on this topic for more information.
Take Action – Hormones for Menopause
The best action you can take is to arm yourself with accurate information about menopause and hormone therapy. There are good resources that can be helpful to understand the facts about menopause and research on hormone replacement. See Additional Resources below for more information.
Discuss menopause and hormone treatment with your physician, keeping in mind that you may have to search for a physician who has training and experience in this area. In the U.S., you can check the North American Menopause Society’s website for trained providers.
Don’t assume that menopause hormone treatment is out of the question if you have been diagnosed with breast cancer. It’s critical to evaluate your risks vs the benefits of hormone replacement therapy with your physician.
Additional Resources
Websites with more information
- Hormonally.org
- North American Menopause Society
- Let’s Talk Menopause
- The Menopause Charity
- Newson Health Menopause Society
- Women Living Better
Books and Media
- Estrogen Matters by Dr. Avrum Bluming and Carol Tavris, 2018
- The Menopause Manifesto by Dr. Jen Gunter, 2021
- Non-profit to address gaps in women’s health education by Sorina Mihaila, Femtech World, May 1, 2024
- Preparing for the Perimenopause and Menopause by Dr. Louise Newson, 2021
Select publications
- Batur P, Blixen CE, Moore HCF, Thacker HL, Xu M. (2006). Menopausal hormone therapy (HT) in patients with breast cancer. Maturitas 53 (2006) 123–132. (Full text).
- Bluming A. (2022). Hormone replacement therapy after breast cancer: It is time. Cancer J 28(3):p 183-190. (Full text).
- Cold S, Cold F, Jensen M-B, et al. (2022). Systemic or vaginal hormone therapy after early breast cancer: A Danish observational cohort study. J Natl Cancer Inst 114(10):1347-1354. (Full text).
- Davis SR, Pinkerton J, Santoro N, et al. (2023). Menopause—Biology, consequences, supportive care, and therapeutic options. Cell Sept. 5. (Full text).
- Dimitrakakis C, Jones RA, Liu A, Bondy CA. (2004). Breast cancer incidence in postmenopausal women using testosterone in addition to usual hormone therapy. Menopause 11(5):p 531-535. (Abstract).
- Hodis HN, Mack WJ. (2022). Menopausal hormone replacement therapy and reduction of all-cause mortality and cardiovascular disease: It is about time and timing. Cancer J 28(3):208-223. (Full text).
- Glaser R, Dimitrakakis C. (2013). Testosterone therapy in women: Myths and misconceptions. Maturitas 74(3):230-234. (Full text).
- Laing AJ, Newson L, Simon JA. (2022) Individual benefits and risks of intravaginal estrogen and systemic testosterone in the management of women in the menopause, with a discussion of any associated risks for cancer development. Cancer J 28(3):p 196-203. (Abstract)
- North American Menopause Society (2022). The 2022 hormone therapy position statement of The North American Menopause Society. (Free text).
- Panay N, Fenton A. (2009) The role of testosterone in women. Climacteric 12:3,185 — 187. (Editorial)
- Stuursma A, Lanjouw L, Idema DM et al. (2022). Surgical menopause and bilateral oophorectomy: Effect of estrogen-progesterone and testosterone replacement therapy on psychological well-being and sexual functioning; A systematic literature review. J Sexual Med
19(12) 1778-1789. (Free text). - Vinogradova Y, Coupland C, Hippisley-Cox J. (2019). Use of hormone replacement therapy and risk of venous thromboembolism: nested case-control studies using the QResearch and CPRD databases. BMJ. 364: k4810. (Full text).
- Last updated on October 17, 2024
Tell us what you think
Human Health News

Hormone therapy is safe for treating menopause symptoms
Many women approaching menopause are concerned about the safety of hormone therapy. That’s because in 2002, researchers reported that hormone replacement therapy — or HRT — was related to increased risk of breast cancer. However, experts now report that hormone therapy in early menopause is safe and beneficial.

Targeting 14 risk factors can cut dementia cases by nearly half
As life expectancy increases worldwide, more people are living with dementia. Even though the age-specific rate of dementia is falling in some high-income countries, the overall number of cases is still rising. This highlights the need for effective prevention strategies. The Lancet Commission on dementia prevention, intervention, and care recently updated its findings, revealing 14 modifiable risk factors that can help reduce dementia cases. Their latest report emphasizes that targeting 14 risk factors can cut dementia cases by nearly half.
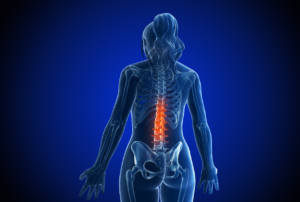
Estrogen and low back pain: what the research shows
Low back pain is a common problem that affects millions of people worldwide — especially older women. While the causes of low back pain can be varied, new research suggests that estrogen may play a role in its development and severity. A recent review published in Bone Research reported that estrogen receptors are present in the intervertebral discs and facet joints. These two key areas of the spine are often affected by low back pain. This suggests that estrogen may have a direct impact on the health of these tissues.

Hormone therapy is safe for treating menopause symptoms
Many women approaching menopause are concerned about the safety of hormone therapy. That’s because in 2002, researchers reported that hormone replacement therapy — or HRT — was related to increased risk of breast cancer. However, experts now report that hormone therapy in early menopause is safe and beneficial.

Targeting 14 risk factors can cut dementia cases by nearly half
As life expectancy increases worldwide, more people are living with dementia. Even though the age-specific rate of dementia is falling in some high-income countries, the overall number of cases is still rising. This highlights the need for effective prevention strategies. The Lancet Commission on dementia prevention, intervention, and care recently updated its findings, revealing 14 modifiable risk factors that can help reduce dementia cases. Their latest report emphasizes that targeting 14 risk factors can cut dementia cases by nearly half.
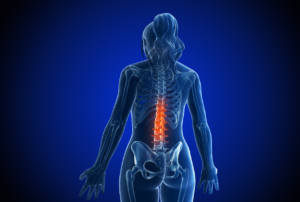
Estrogen and low back pain: what the research shows
Low back pain is a common problem that affects millions of people worldwide — especially older women. While the causes of low back pain can be varied, new research suggests that estrogen may play a role in its development and severity. A recent review published in Bone Research reported that estrogen receptors are present in the intervertebral discs and facet joints. These two key areas of the spine are often affected by low back pain. This suggests that estrogen may have a direct impact on the health of these tissues.

Links between sleep, Alzheimer’s disease, and sex differences
Did you know that women are more likely to develop Alzheimer’s disease than men? In fact, about two-thirds of Alzheimer’s cases in the U.S. affect women. One key factor that might help explain this disparity is the connection between sleep disruptions, Alzheimer’s disease, and sex differences. As a recent study shows, it’s becoming clear that sleep problems, especially during and after menopause, may play a significant role in women’s increased risk for Alzheimer’s.