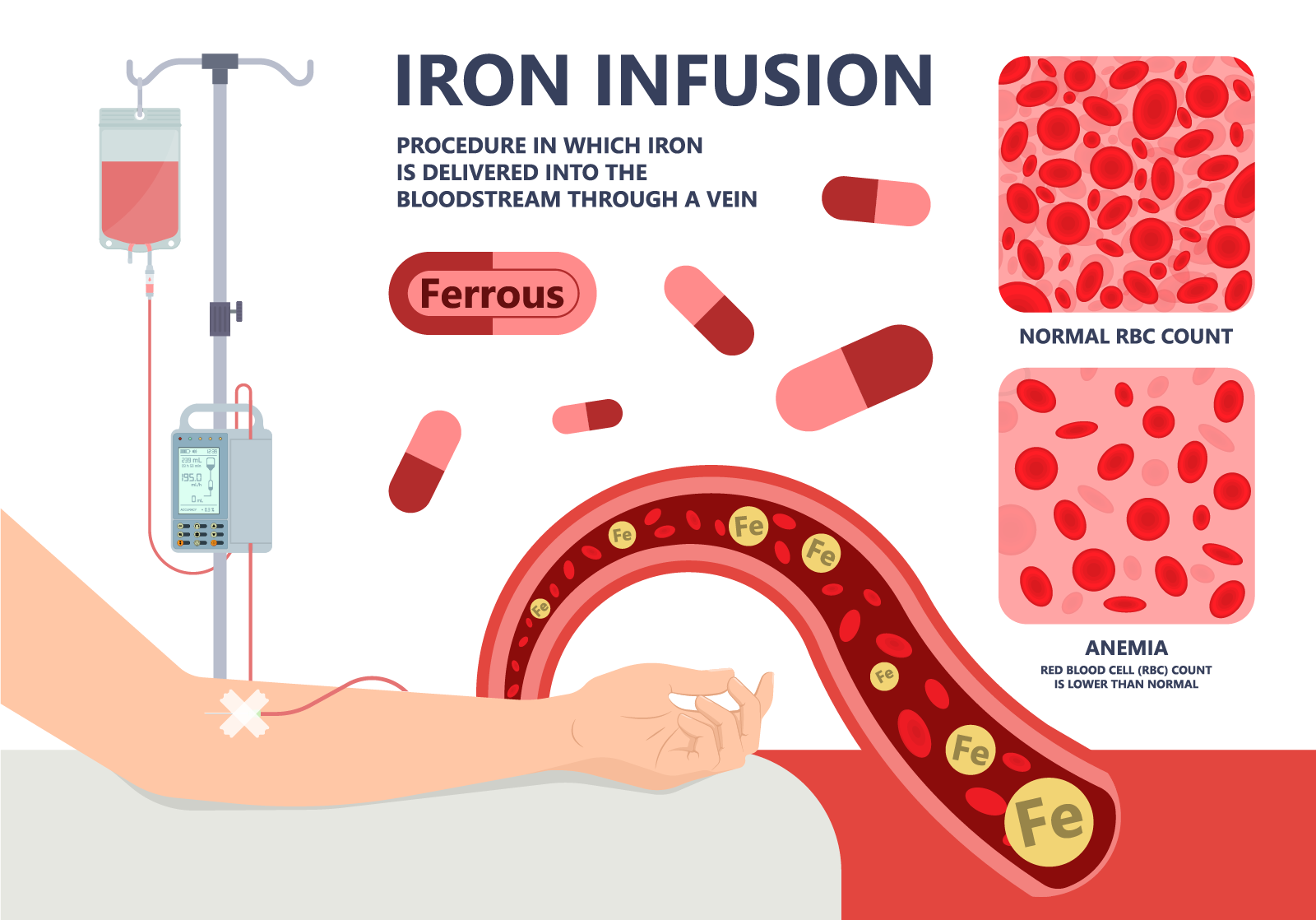
Iron deficiency and anemia are commonly diagnosed and can result in significant negative health impacts if not treated. Intravenous iron offers a rapid treatment option that is often superior to oral iron.
Looking for an infusion center?
Check this infusion center website locator.