Overused, unnecessary, or low-value healthcare options can have significant negative effects on patients, providers, and the healthcare system. This is partly due to cascading effects from an initial low-value test or procedure. A recent study in JAMA Network reported on the frequency and downstream financial impact of low-value PSA (prostate specific antigen) testing for prostate cancer.
What is low-value healthcare?
“Low-value” tests or procedures provide no or minimal benefit to patients in specific clinical situations, but can incur risks. This does not mean that the tests or procedures should never be used. They are just considered low-value when overused or unnecessary for a specific patient.
As an evidence-based health education resource, the Parsemus Foundation promotes healthcare literacy and empowerment. A long-term goal has been to shed the light on overused medical procedures. The foundation has helped to shed light on these overused, low-value tests and procedures since 2010. Since then, healthcare professionals have been identifying them and the results are often published in medical society journals. Yet, for many reasons, clinicians often continue to recommend low-value, overused medical tests and procedures. For example, according to the Lowns Institute, coronary stents were used unnecessarily in 22% of the cases studied from 2019-2022. This is despite recognition that stents were overused since the 2010 “Less is More” feature of JAMA Internal Medicine.
However, there has been some progress in reducing low-value healthcare. Choosing Wisely helped to move the conversation forward between patients and clinicians about which tests are needed and which are not. They report over 700 recommendations from medical specialty societies for tests and treatments they said were overused or unnecessary.
Cascading treatment effects
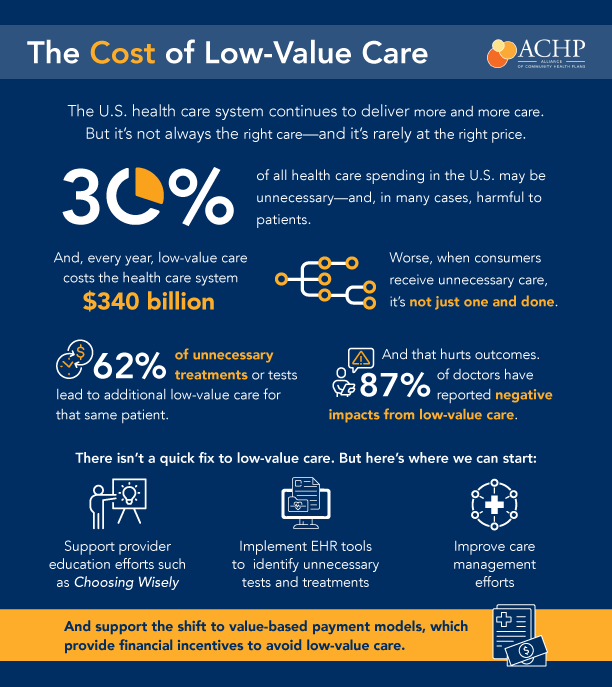
An evaluation of the impacts of 626 low-value services recognized by Choosing Wisely was conducted in the United States. The study included the concept of “cascading effects”. These effects involve downstream medical services of uncertain value that follow from an initial test or treatment for an individual patient. They include follow-up testing or treatment after an unclear or abnormal finding from prior service. In this study, cascade potential was defined based on the likelihood of incidental findings, overdiagnosis, false positive results, or cascading adverse events.
The researchers reported that almost half of the low-value services had high potential for direct harm and 62% had high potential for cascading effects. Three of the low-value services identified by Choosing Wisley were concerning on every measure. They were high cost, used in the general population, had high risk of direct harm, and high cascade potential.
Low-Value PSA Test for Prostate Cancer Screening
Researchers from Tufts Medical School recently conducted a study evaluating cascading effects of the prostate-specific antigen (PSA) tests for prostate cancer screening. The study focused on the frequency of use and cost of care cascades of the PSA test used for 70+ year old men without any symptoms. Records for over 995,000 men enrolled in the Medicare Advantage plan were evaluated.
The results were troubling. First, 39% of the men in the study received the low-value cancer screening despite the PSA test being discouraged for this population of patients by multiple guidelines. Additionally, cascading effects were common, with 63% of men receiving follow-up care including additional PSA tests. For every $1 spent on a low-value PSA cancer screening, an additional $6 was spent on care cascades.
In conclusion, the authors recommended reforms to reduce initial low-value healthcare and avoidable care cascades. This would help to decrease harm, enhance equity, and improve health care efficiency.
What can you do about low-value care?
Medical societies can encourage adherence to care guidelines among physicians and the healthcare system. But it’s also important for each patient to fully understand any recommended tests or procedures. Ask questions about the test or procedure and understand any risks by speaking openly to your healthcare provider. You can also do your own research to learn more about a recommended test or procedures. With misinformation common in online resources, be sure to use evidence-based information when searching the internet. Some tips can be found here.